RFK Jr. Guts the ACIP: What's Next?
Federal vaccine policy is changing rapidly, which could have varying effects at the state and local level.
The vaccines policy world is quite small - so, by now, most everyone knows that the Advisory Committee on Immunization Practices (ACIP) was made entirely new by Secretary of Health and Human Services (HHS) RFK Jr., who unilaterally terminated the 17-member roster in favor of 8 new hand-picked voting members. Concerns about this move range widely, from concerns about the members themselves (who, at best, collectively lack vaccines expertise; at worst, they include proud “anti-vaxxers”) to the politicization of a long-standing, evidence-based vaccine policymaking process.
Most notably, given RFK Jr.’s stated intent to “examine” the childhood immunization schedule and recent decisions to remove COVID-19 vaccine recommendations for healthy children and pregnant people, many are concerned this new ACIP roster could revisit existing recommendations and possibly remove them.
ACIP recommendations are not binding - that is, no one is mandated to get a vaccination if it’s recommended by the Committee. However, several federal laws link ACIP recommendations to insurance coverage without cost sharing (my Avalere Health colleagues and I summed these up in 2023). As a result, without these recommendations, people seeking vaccination could be required to pay for it out-of-pocket. This is often a prohibitive barrier, as we saw in 2023 when adult RSV vaccines first rolled out to the public - eligible people who were told they’d have to pay simply left, facing up-front costs of more than $300.
So, if the new ACIP revisits and decides to remove certain vaccine recommendations, who could be most affected?
This is a complicated question - there are so many factors that affect a person’s ability or willingness to get a vaccine. Several studies observe higher vaccination rates for people with insurance coverage than for people without it. In this case, though, we could be looking at the removal of required coverage for certain vaccines, and so insurance coverage may no longer be a deciding factor.
Further, certain populations may be worse off by remaining unvaccinated than others. For example, one study found that higher socioeconomic status correlated with higher influenza vaccination rates; another study found that lower socioeconomic status was also correlated with lower HPV vaccination. Compounding this are several studies that found increased influenza-related hospitalizations in neighborhoods with lower socioeconomic status (e.g., Connecticut, Tennessee).
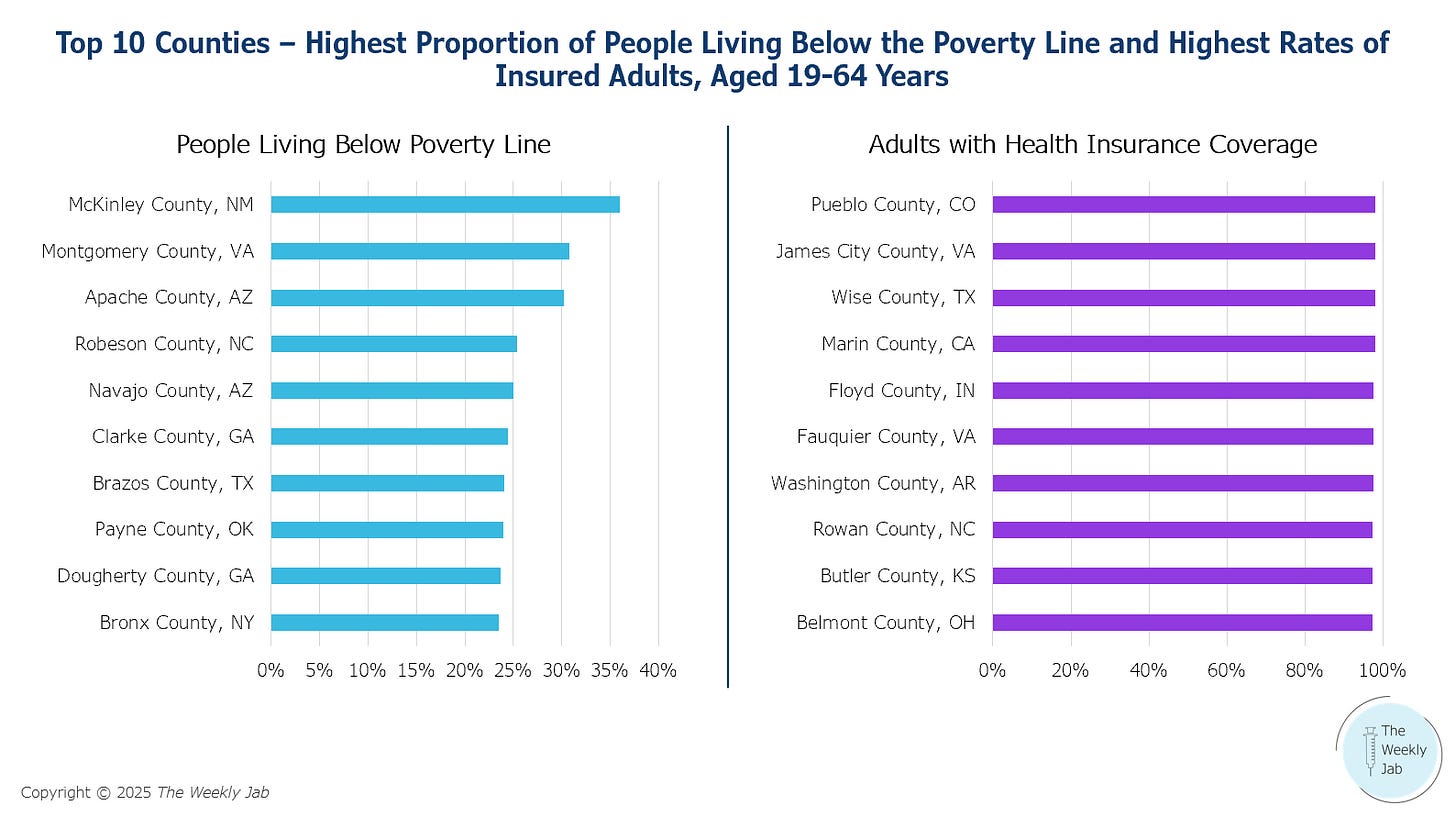
To understand where in the US people could be most affected by the removal of ACIP recommendations, I dug into 2023 American Community Survey (ACS) data for two things: 1) which counties in the US had the highest proportion of people living below the poverty line and 2) which counties in the US had the highest rates of insured adults.
Note - I chose to focus on adults, since many children are eligible for free vaccines through the Vaccines for Children (VFC) program. VFC has its own ties to the ACIP, but it’s a bit more complicated - keep an eye out for my take on this next week.
What does the ACS data show us?
Not surprisingly, there is very little overlap between counties with the highest proportion of people living below the poverty line and counties with the highest insured rates - in 2023, 20.2% of people living below the poverty line were uninsured, 10.7% higher than the national average.
The first thing I wanted to look at was the types of insurance coverage represented in counties with the highest rates of insured adults. My goal was to understand how the removal of ACIP recommendations could affect coverage mandates based on the federal statutes associated with each coverage type.
Highest Insured Rate - Pueblo County, Colorado
There were just over 88,000 insured adults aged 19-64 years in Pueblo County, Colorado in 2023, representing 98.1% of the people in this age group. More than half of this group (61.7%) had some type of private insurance; the vast majority of this segment (91.3%) had employer-sponsored coverage. Of the 28.6% of people with public insurance coverage, most (83.1%) were covered by Medicaid or another form of means-tested public coverage.
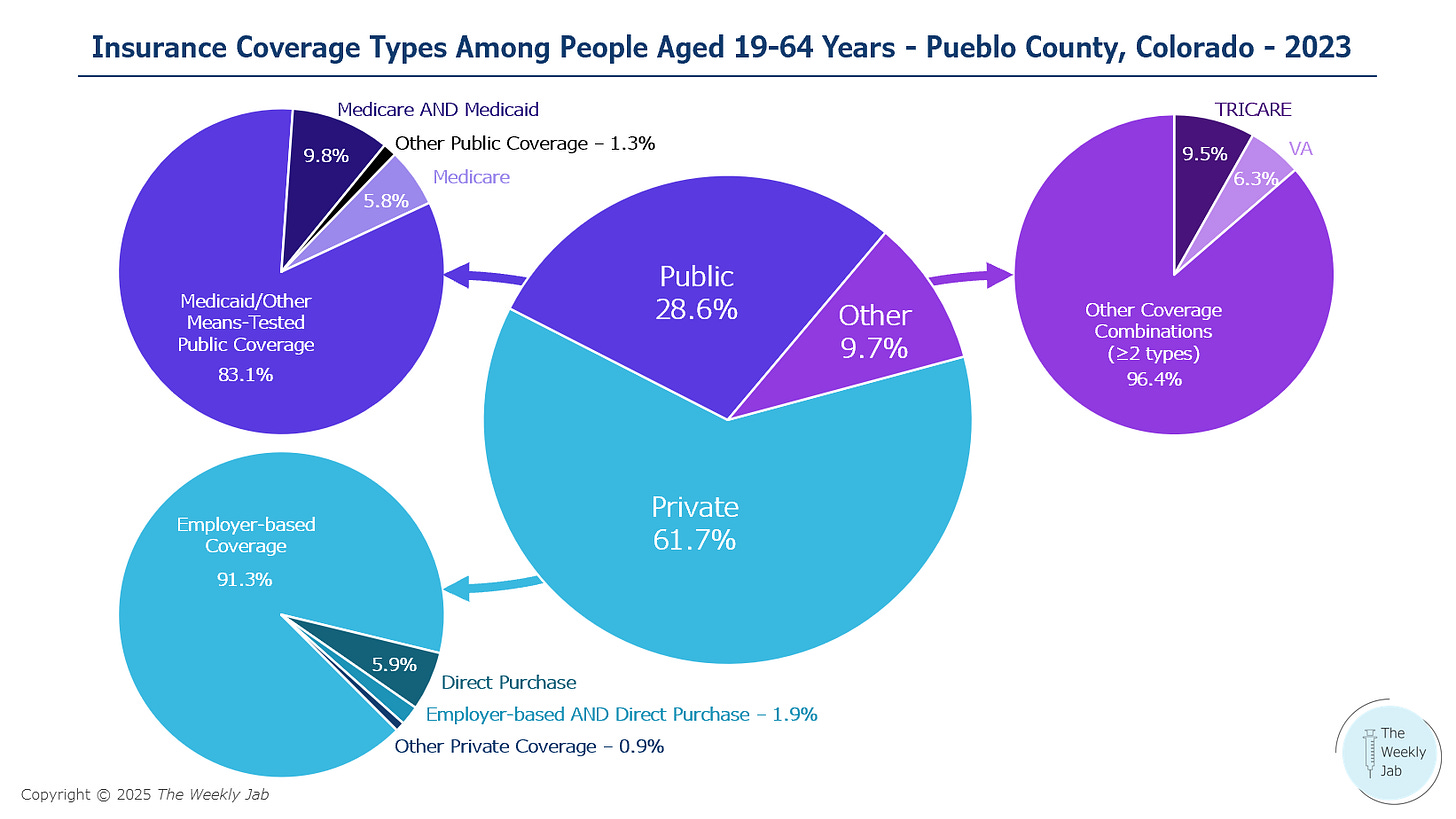
There are different laws, regulations, and sub-regulatory guidance at play that mandate coverage without cost sharing for vaccines - most of which is tied to ACIP recommendations - for each type of insurance coverage. In summary, without ACIP recommendations, vaccine coverage would be up to the discretion of payers and programs across most markets, potentially resulting in most of Pueblo County’s population of adults aged 19-64 years losing mandatory $0 coverage for vaccines.
Table 1 - Federal Laws Governing $0 Vaccine Coverage by Insurance Market
For those who do lose vaccine coverage, paying for a vaccine out-of-pocket remains an option. While this is not a viable option for many people, it could be more likely to occur in Pueblo County, where most of the adult residents have incomes at or above the federal poverty level, than in other counties where this rate is much lower. McKinley County, New Mexico is one such county - in 2023, 35.9% of adults aged 20-64 years had incomes below the federal poverty level. About 86% of this population had health insurance, and while there is no ACS data on coverage types in this county, it is likely that any loss of $0 vaccine coverage could have a greater impact on this county’s insured population than on adults in counties like Pueblo.
What else could change with the potential removal of ACIP recommendations?
Beyond insurance coverage, other policies could limit access to vaccines even for those that choose to pay for them out-of-pocket. Specifically, state laws and regulations govern 1) whether vaccines can be administered in pharmacies, 2) the specific vaccines authorized for administration, 3) which provider types can administer them, and 4) to whom they can be administered. These pharmacy scope-of-practice laws vary by state, and some states tie scope-of-practice to ACIP recommendations. For example, going back to the counties referenced above - Pueblo County, Colorado, and McKinley County, New Mexico - we see key differences in their state laws that could affect pharmacy vaccine access.
Table 2 - Colorado and New Mexico Scope-of-Practice Laws and Regulations
Of note, in the event of an ACIP recommendation removal, New Mexico has a kind of “failsafe” built into its policies that Colorado does not; therefore, it is more likely that pharmacy vaccine access could be maintained in New Mexico vs. a state like Colorado.
Anticipating this scenario, several state legislatures sought to pass laws in their most recent sessions providing alternatives to ACIP recommendations that could maintain continuous coverage for vaccines without cost sharing. In hindsight, those efforts were well founded. One example is Maryland House Bill 974, enacted on May 20, which mandates the state’s Health Commissioner to enforce coverage requirements for vaccines and preventive services in accordance with federal “recommendations and guidelines in effect on December 31, 2024” and further authorizes the Commissioner to adopt additional regulations to “enhance the scope of preventive services.” Essentially, this new law freezes ACIP recommendations at a point in time, allowing the state to issue its own regulations for vaccines approved at a later date.
What could we expect going forward?
We may get more clarity after this week’s ACIP meeting - the first meeting to feature RFK Jr.’s new cast of characters. That said, given some of this year’s state legislative activity and unique, county-specific vaccine access challenges, we could see more fragmented vaccine policies at the state and local level. There are also several highly qualified expert bodies who could fill the void - medical societies like the American Academy of Pediatrics and the American Academy of Family Physicians, and the newly established Vaccine Integrity Project - so state governments may coalesce around any or all of these groups. Whatever it is, a concerted, organized effort to adapt to the shifting federal landscape is crucial to limiting the number of people who lose access to life-saving vaccinations.